Malaria diagnostic resistance: implications for endemic regions and global treatment programmes
Matthew Spencer is a fifth-year medical student from UCL who is interested in a career in infectious diseases and tropical health. He was the winner of the RSTMH Medical Student Essay Competition 2018, for the essay he has adapted below. Matthew received the award and prize at our Topics in Infection in January, part of which was the book "Light out of deep darkness: A biography of Arthur Ferguson MacCallan, the trachoma pioneer", written by his grandson Michael MacCallan.
Why malaria matters
Despite decades of concerted international efforts, malaria is still a global health burden. Plasmodium falciparum is the commonest and deadliest malaria species.
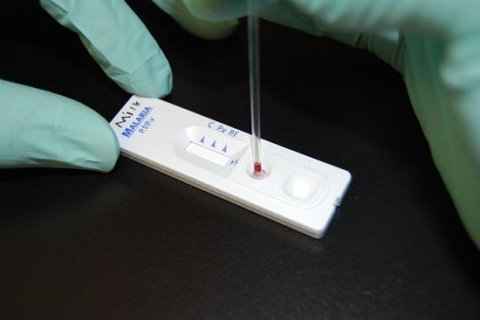
Diagnosis and treatment of malaria has been transformed by the rapid diagnostic test (RDT). These are cheaper and require little of the infrastructure and expertise necessary for microscopy diagnosis. The commonest RDT detects P. falciparum histidine rich protein 2 (pfHRP2).
In primary studies, this test demonstrated high levels of consistency and performance.(1) In areas of high endemicity, pfHRP2 RDTs are the backbone of clinical malaria management. (WHO, 2018)
The rapid diagnostic test
RDTs are highly specific for their protein of choice. The ability of pfHRP2 RDTs to function therefore relies on pfHRP2 being present in P.falciparum’s genome and being translated into a protein.
The global malaria research community has been shocked by recent studies that describe radically impaired sensitivity of the pfHRP2 RDT compared with studies only one decade before.(2)
Given the widespread usage of pfHRP2 RDTs in malaria diagnosis, it is essential to ascertain the cause of reductions in sensitivity and false negative results.
Misdiagnosis of malaria due to pfHRP2 deletions has led to delays in treatment and could cause increased mortality from the disease.(3) Several suggestions have been made as to why pfHRP2 RDT sensitivity has decreased.
Alterations in pfHRP2 genome
One hypothesis put forward for the cause of false negative RDTs is the loss of the pfHRP2 gene from the plasmodium genome. During research for a WHO RDT evaluation programme,(2) it was found some patients who were positive for P.falciparum based on microscopy tested negative on a pfHRP2 RDT.
PCR was then used to confirm loss of pfHRP2 and pfHRP3 genes, while ELISA showed a lack of pfHRP2/pfHRP3 protein expression. pfHRP3 is another malaria antigen used in malaria RDTs.
41% of samples were shown to lack pfHRP2, and 70% lacked pfHRP3. Subsequent studies in Brazil, clearly separated in time and place from sub-Saharan Africa, have reproduced this finding.(4) Interestingly, Maltha and colleagues also found that two false negative strains of P. falciparum did not have pfHRP2 deleted but still tested negative on RDT.
The authors hypothesise that a mutation or deletion in strains with pfHRP2 present might have altered the binding of RDT antibody to pfHRP2 antigen, and so have led to false negatives.
This hypothesis was explored previously(5), with analysis finding certain pfHRP2 sequences could be detected at low parasitaemia (<250 parasites/ μl, while other could not, but no variation at higher levels of parasitaemia. Many of the sequences used came from laboratory lines and not field isolates. In a subsequent study(6), no relationship was found between the pfHRP2 gene sequence and RDT detection rate for P. falciparum even at low parasitaemia. Subsequent studies (7) have also analysed pfHRP2 sequences and found no link between pfHRP2 RDT positivity and pfHRP2 sequence.
The most likely explanation for false negative RDT results therefore appears to be gene deletions, due to the wide variety of reports in the literature that show microscopy positive, RDT negative test subjects with deletions of pfHRP2. As well as the aforementioned studies in Peru, studies in Brazil (3), Mali (8), Eritrea (9), Rwanda (10) and India (11) have corroborated that pfHRP2 deletions occur and cause false negative results.
The prozone effect
Another explanation of false negative pfHRP2 RDTs is a prozone-like effect. Studies show increasing quantities of pfHRP2 eventually lead to a reduction in the intensity of the line indicating a person is malaria positive, although the line does not vanish.(12)
It is possible therefore, that an RDT may be interpreted incorrectly due to a reduction in line intensity. Other studies have found a prozone effect in 16 of 17 pfHRP2 RDTs tested, but no such effect for RDTs testing other proteins.(13)
The prozone effect can therefore account for reductions in line intensity, but this would rely on this effect only causing issues since pfHRP2 deletions began to occur, as it has not previously caused issues. Furthermore, an increasing prozone effect would mean that parasite levels in the bloodstream have been increasing worldwide, to levels that seem unlikely.(12)
As mentioned in the above studies, line visibility would not be an issue except in extremely high parasitaemias, combined with user error. These are both relatively rare occurrences and so for them to account for the majority of false negative pfHRP2 RDTs seems unlikely.
Why is pfHRP2 being deleted?
The cause for mutations occurring is unclear, but it could be an evolutionary mechanism to overcome the selection pressure of RDTs. If a patient does not test positive, they will not receive treatment, and the parasite can continue to reproduce.
It would therefore be expected that P. falciparum strains with a pfHRP2 deletion would have a survival advantage and therefore be more likely to reproduce and increase in number. The deletions likely existed before RDT’s development and have only proved advantageous since their widespread usage.
The origins and causes of increasing pfHRP2 RDT negative malaria strains in Peru has been investigated.(14) It was found that the prevalence of pfHRP2 deletions has increased 2001-2005. This suggests a selection pressure for pfHRP2 to be deleted but could not be confirmed from the study.
Furthermore, the deletion of pfHRP2 was not a one-off event, but occurred multiple times in Peru. The authors point out however that RDTs were rarely used in Peru at the time due to the wide availability of microscopy.
One study however is not definitive, and it would be of interest to see further studies analysing pfHRP2 prevalence and origins in different areas.
Key to understanding why pfHRP2 is being deleted will be finding the protein’s function. There appears to be no survival advantage by modifying the protein, however due to its subteloromic location it mutates frequently.(6)
More work is therefore needed to understand the function of pfHRP2 and why it can mutate so much without any loss of survival fitness.
Solutions to decreased pfHRP2 sensitivity
Problems of resistance typically apply to treatment rather than an investigation. Organisms will always adapt to selection pressures exerted on them, and so it is unsurprising to see the prevalence of pfHRP2 deletions increasing in the P.falciparum genome due to the proteins use in an RDT.
Solutions used to treatment resistance in HIV medicine rely on combining multiple treatments together, known as highly active anti-retroviral therapy (HAART).
Perhaps combining multiple RDTs would allow increased sensitivity in detecting P. falciparum than with one RDT alone. A candidate to combine with pfHRP2 would be the lactate dehydrogenase protein (LDH).
LDH is produced by all human infecting malaria species (15) and so can detect species besides P. falciparum. A systematic review comparing LDH and pfHRP2 RDTs for diagnosis of P. falciparum found that LDH RDTs were more specific, and pfHRP2s more sensitive.(16)
Sensitivity and specificity has been shown to be higher when pfHRP2 and LDH RDTs are combined. In addition, the LDH RDT picked up 53% of pfHRP2 negative samples which tested negative on pfHRP2 RDTs.
This shows that combination RDTs can be more effective than either alone, and perhaps provide a solution to the pfHRP2 deletion problem.
Another candidate to replace the single RDT is whole genome PCR testing. A key feature of the malaria genome would be used as a primer, ensuring the parasite could not mutate to avoid detection.
PCR is more sensitive than microscopy or RDT (17) and can detect ultra low levels of parasitaemia. Currently logistical issues prevent PCR being used in place of other methods, but these barriers will reduce over time, and allow PCR to be used commonly.
Future questions and conclusion
Several unanswered questions emerge from deletions in pfHRP2. The cause, although speculated to be due to pfHRP2 RDT introduction, is unclear.
The function of pfHRP2 also remains unclear, and so it is difficult to hypothesise the causes of deletion prevalence increasing. Additionally, some patients testing false negative on pfHRP2 RDT had no deletion in the gene. This would seem to indicate factors apart from deletions of the pfHRP2 gene are at play.
These questions need to be answered quickly, as over 150 million RDTs are carried out annually in Sub-Saharan Africa alone. Aside from causing an increased malaria burden, false negative malaria testing would cause economic consequences as patients require hospital admissions following more severe infections.
It is perhaps pertinent to ask whether the focus on a universal test has provided an ideal situation for the parasite, which can use evolution to overcome the selection pressure of an RDT, and whether having a wider range of investigations is more useful for organisms capable of evolving.
This question applies to other infectious diseases relying heavily on a single diagnostic tool, such as GeneExpert for TB diagnosis in Sub-Saharan Africa.
In conclusion, the decreasing sensitivity of pfHRP2 RDTs is likely to be due to deletions of the gene from P. falciparum’s genome. New approaches may include combined RDTs and PCR, however there will never be a perfect investigation as the parasite will always evolve to combat a selection pressure.
Ultimately, it is not possible to prevent malaria and other infectious organisms from evolving, as this is their nature. What is necessary however is the ability for healthcare professionals and researchers to adapt to the changes that occur and come up with novel solutions to the problems they face.