The globally expanding dengue problem
Dengue viruses can cause a range of conditions from asymptomatic infection, self-limiting febrile illness, potentially fatal plasma leakage syndrome to severe neurologic, cardiac, renal or other organ dysfunction. The primary vector for dengue is the day-biting female Aedes agypti mosquito. There are four distinct dengue serotypes; infection with one serotype generally results in long-term homotypic immunity but only short-term heterotypic protection, such that repeat dengue infections can occur.
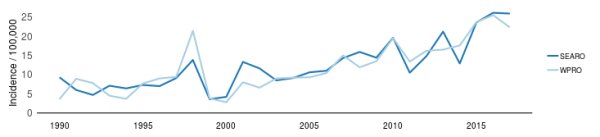
The most affected countries are in tropical Asia and Latin America. The WHO calculates the yearly incidence of dengue based on the number of clinically-suspected and laboratory-confirmed cases officially reported from Ministries of Health (Figure 1).
Although these data provide an incomplete assessment of the global burden of dengue disease because of underreporting or misclassification, they are useful for understanding the overall trend, as well as periodic outbreaks of the disease.
The Global burden of Disease study estimated that the number of apparent dengue cases increased from 8 million (3 to 17 million) in 1990 to 58 million (24 to 122 million) in 2013.
There has also been a worldwide expansion of dengue endemicity. Ongoing global urbanisation, climate change, travel and enlargement of the Aedes range have led to predictions that dengue will further intensify in already endemic countries and extend to new geographic areas. Within this overall increasing trend, there are seasonal and yearly variations in the occurrence of dengue. Interestingly, the outbreak patterns in the SEARO, WPRO and PAHO countries (Figure 1) show remarkable similarities.
Low incidence periods followed by large epidemics every three to five years have been attributed to annual climate variability, cross-protection from other flaviviral outbreaks and accumulation of susceptible populations during inter-epidemic periods. The potential contribution of evolutionary shifts in dengue viral lineage is an area of intense investigation.
Following the large Zika epidemic in the Americas, there was a significant reduction in reported dengue cases in 2017-2018. But after this decline, a sharp increase in cases is being observed in 2019 in several Latin American and Asian countries, which is not yet captured in Figure 1.
From February to August 2019, HealthMap showed 2,816 alerts of local or imported dengue from official, newspaper and other media sources (Figure 2). As the rainy season continues in many dengue-endemic countries, increasing numbers of dengue cases are expected.
Implementing wide-scale vector control programmes has been difficult to sustain, particularly in low-income dengue endemic countries. But even high-income countries like Singapore continue to struggle with dengue.
The development of a safe and effective dengue vaccine would be of great benefit but the complex immune response to the dengue virus and the need to induce concomitant protection against its antigenically distinct serotypes pose significant challenges. Although CYD-TDV (Dengvaxia, Sanofi Pasteur) was the first dengue vaccine to become available, its differential performance by dengue seropositivity is a serious set-back. Instead of protecting against all serotypes, the vaccine appears to act like a single dengue infection, making the timing of its administration crucial.
Since there is an increased risk for severe manifestations during secondary dengue, administration of CYD-TDV to seronegative people may increase the risk for severe dengue during the next natural exposure to the virus.
On the other hand, if the person already had a primary dengue infection, CYD-TDV would confer protection against the risk of severe manifestations associated with secondary dengue infections. The WHO recommendation that the vaccine be given only to those who are dengue seropositive requires an affordable, rapid and accurate test of dengue serostatus, which is currently not available. Neutralisation testing is considered the gold standard for ascertaining dengue serostatus but is resource-intensive and only available in research centres.
In the absence of a better vaccine and reliable vector control, avoidance of the day-biting mosquito transmitters and prompt and effective case management (including early assessment, close monitoring and the judicious use of intravenous fluids) are the primary strategies against dengue in endemic countries. Through improved case management, many countries have reduced their dengue case fatality rate to less than 1%.
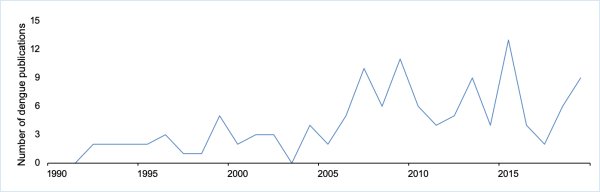
To promote scientific knowledge in this field so as to help address the growing dengue problem, we aim to publish more papers on dengue in RSTMH's jourmal, Transactions. A quick search using “dengue” in the title showed that the number of dengue publications in the Transactions has paralleled the increasing global importance of the disease (Fig 3). In 1990 and 1991, there were no dengue publications in the Transactions identified. From 2002 to 2019, there have been 126, so far, with the numbers varying considerably from year to year (Fig 3).
One of the most read Transactions articles is the highly topical review of dengue diagnostics and implications for surveillance and control. The authors cover a wide range of laboratory methods for the confirmation of acute dengue and for serologic screening prior to vaccination. This is an article of broad public health use and interest.
If you have dengue research that you wish to publish, we invite you to consider submitting your manuscript to Transactions.
Sign up to our newsletter for more updates