Reflections on World TB Day
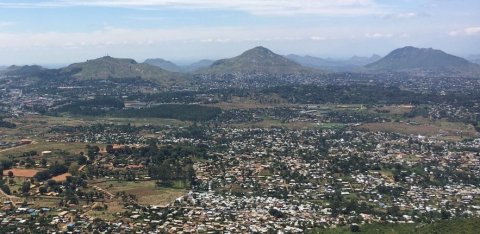
This World TB Day, Dr Rachael Burke, Wellcome Research Fellow, LSHTM and Malawi-Liverpool Wellcome (MLW) Clinical Research programme, Blantyre, Malawi looks at current research into TB after two years of the COVID-19 pandemic.
Today is World TB day, and we are reflecting on the grim reading from the most recent Global TB report. Tuberculosis (TB) deaths have increased for the first time in over a decade, and we are now further away from our goals of ending TB. Driven by the direct and indirect effects of the COVID-19 pandemic, the “diagnostic gap” for people with TB has increased and fewer people are accessing diagnosis and treatment for TB.
More than ever, we need strong, well-led, responsive, “pro-poor” healthcare systems to help people with tuberculosis access the diagnostic, treatment, and care services they need. We also need better tools and strategies to identify people who would benefit from TB testing and accurate and rapid TB screening and diagnostic tools.Research is one of the important building blocks of improving TB services – alongside advocacy, financing, learning from those affected by TB, and health systems leadership. Our TB research team in Malawi is led by this year’s Chalmers Medal recipient, Prof Liz Corbett, building on a lifetime of dedication to clinical services, training and research by the late Prof Malcolm Molyneux and his wife, Prof Liz Molyneux. Our research team does research on TB epidemiology and diagnostics at all levels of healthcare system, with special focus on diagnostic impact evaluations including active case-finding in communities and facility-based systematic screening in hospitals and primary care. We are passionate about working towards ending the TB epidemic!
TB Epidemiology Research
This World TB Day, I am reflecting on what we have learned from TB epidemiology screening, diagnosis, and care research in the past 12 months from Malawi and elsewhere. How could this knowledge help us move onwards, past the devastating effects of COVID on TB?
On the screening side, in the past 12 months, we have had new research-informed guidelines on TB screening from WHO, the results of the large TREATS trial in Zambia and South Africa presented as part of the conference proceedings at the Union for TB and Lung Disease, and the publication of the HomeACF trial.
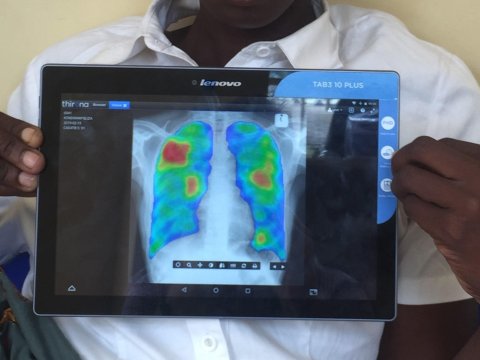
In the WHO screening guidelines launched on World TB day last year, WHO recommends more strongly that TB screening should be undertaken in populations at high risk for TB, with methods that include digital Chest Xray and computer-assisted diagnostics. However, there is a note of caution here, with plenty of evidence that even well-implemented and intensive interventions do not always improve patient-outcomes; TREATS was a large cluster randomised trial in Zambia and South Africa which reported findings in October 2021. TREATS found no evidence that population screening for TB and HIV (using TB symptoms as a first step) made a difference to TB incidence or prevalence. Similarly, the homeACF trial was published in December 2021; this trial evaluated home-based TB/HIV screening for household contacts of people with TB in South Africa. HomeACF showed that the household screening intervention didn’t reduce incident TB or death compared to a referral letter.
From the perspective of diagnostic tests, we were delighted to see in the WHO TB screening guidelines the recommendation for the first time that Digital Chest X-ray with Computer Aided Diagnosis could be used for screening. This builds on Peter MacPherson’s PROSPECT trial, published in September 2021, showing that TB screening in Malawi using Computer Aided Diagnosis increased the timeliness of TB diagnosis in primary care. We are close to completing the CASTLE trial using chest X-ray and Computer Aided Diagnosis among adults living with HIV in hospital.
Novel TB diagnostic tests are undergoing evaluation; we have been partners in evaluating new urine diagnostic tests and blood based “host response” tests.
From the health systems perspective, our team in Malawi with our National TB Programme and District Health team partners, were able to capture the impact of COVID-19 on Tuberculosis notifications. In July 2021, we published an observational study showing an immediate 36% reduction in people diagnosed with TB at the start of the COVID-19 pandemic in Malawi. However, we were pleased to see that TB notifications recovered fairly quickly after the initial shock. Others have done similar excellent epidemiology work.
The way forward
What is the way forward and how to we get past these present COVID-19 shocks, to ensure that people with TB can access the diagnosis, treatment, and care services they need? I was inspired by some of the work from UNAIDS about how HIV service and COVID-19 response can learn from each other, particularly about “reimagining health services”. They point out the attributes needed for responding to new threats (such as COVID) are largely the same as are needed for responding well to HIV and TB. They highlight flexibility, innovation, equity, tailoring services for the most vulnerable, capacity to synergize biomedical and non-health interventions and a sufficiently data-drive approach. Elsewhere in the documents, the need to involve communities as innovative pioneers is highlighted – which is surely key.
As researchers, we try to identify and highlight what approaches might work best for a renewed effort to close the TB diagnostic gap. I am excited about optimising new diagnostic tools, including digital chest X-ray and excited to see what research is produced in the next 12 months. Even the negative trial findings highlighted above are so critically important, showing how much we need dispassionate evaluation of benefits, harms and opportunity costs of even the most promising-looking new diagnostics, in order to avoid wasteful investments that do not help those in most need. Having spent a lot of time in the past 12 months thinking about TB screening and reflecting on the results of TREATS and homeACF, I think part of the answer is that we need to ensure that there are many routes to accessing TB diagnosis and that these are all equitable and pro-poor. While community based or mobile TB diagnostic facilities may have a role, we should be seeking to outcompete the need for such interventions through, respectful facility-based routine TB diagnosis, treatment and care services that deliver efficient patient-centered early diagnosis for all.
TB services have long been integrated with HIV services, but people with other co-morbid conditions are less well served, and we also need better care and support for people with symptoms identified at TB screening who have conditions other than TB. To this end, I was excited by several ongoing research projects presented at the Wellcome Trust Bloomsbury meeting in Zimbabwe - where I had the pleasure to meet RSTMH President, Prof Gail Davey. There, I learned about person-centred approaches that addressed multi-morbidity and health systems strengthening and a symptom-based (rather than condition-based) approach to diverse conditions of lung health, skin conditions and mental health.
As ever, good research is only one part of what is needed to achieve the change we seek. And my hope is that effective research plus engagement and empowered communities, and health systems will get us closer to EndTB goals by World TB Day in 2023.
