Outbreak of novel coronavirus from Wuhan – an emergency in China with pandemic potential
The rapidly developing outbreak of novel coronavirus infection that started in Wuhan, China is generating considerable international concern. Early comparisons were drawn with the SARS coronavirus outbreak from 2002-2003 that resulted in over 8,000 cases and 774 deaths in 37 countries, but this may be much harder to control. A rapidly convened emergency committee in WHO has decided that a declaration of a Public Health Emergency of International Concern (PHEIC) is not yet warranted, although this was a split decision and it will convene again in five days or earlier. While a PHEIC is a binary decision, many recognise pandemic risk warning signs and agree a coordinated international response is required.
Evolution in Wuhan China
On 12 December 2019, 27 cases of viral pneumonia including seven critically ill patients were reported from Wuhan, a city of 11 million people in central China. The WHO were notified of the outbreak on 31 December and on 9 January 2020 a novel coronavirus was detected through high-throughput sequencing (2019-nCoV). This compares to the delay of six months until SARS-CoV was identified. As 27 January up to 3,000 cases have been reported with 81 deaths, and while limited data exist on the natural history of the disease, early reports suggest that severe disease occurs in 25% of patients, and that fatal cases are older and have significant comorbidities. An epidemiological curve is currently being generated by WHO from data provided by China.
The first epidemiological reports suggested that most of the early cases had links with Huanan Seafood Market in Wuhan that also sells poultry, snakes and bats. Samples from the market have tested positive for 2019-nCoV and phylogenetic analysis has suggested a recent common ancestor virus and a spill-over event from bats. This investigation is ongoing and while it has important implications for disease control, confirmation of human to human transmission mainly occurring in family clusters has generated more concern. The infection of healthcare workers and of nosocomial amplification re-enforces the need for rapid detection, isolation and appropriate infection prevention and control precautions.
International spread
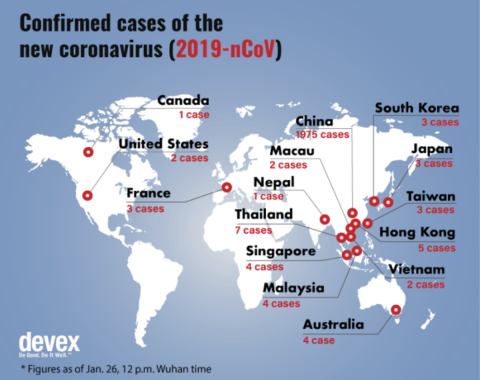
29 provinces in China have now reported cases of 2019-nCoV infection and it is not surprising that cases have been exported to 12 other countries, given the rapid increase in international travel from China since SARS-CoV. This has resulted in increased surveillance activities at ports of entry and extensive travel restrictions have been introduced in Wuhan and other Chinese cities. Restriction of movement is not an intervention that is generally advocated by WHO, but it recognises the autonomy of member states. During various timepoints during the West African Ebola outbreak, travel restrictions were also introduced, and their success has been debated.
It may be that China considers these to be short-term solution to buy time for a comprehensive public health response to be put in place. What is clear however, is that the cooperation and social mobilisation of communities in outbreak affected areas is a key pillar of the response. The current cases that have been managed outside of China are in countries with robust public health infrastructure, but if the outbreak extends to lower and middle-income countries a more coordinated and extensive international response will be required.
Disease transmission
Coronavirus are a large family of viruses, some of which cause common cold while others have resulted in more severe disease such as SARS-CoV or MERS-CoV. The incubation period is currently thought to be 5–6 days, with a range of 2–14 days. The R0 is a key figure and while this varies during an outbreak, early predictions of the R0 in Wuhan are 1.4–2.5, higher than for SARS-CoV and MERS-CoV. While the mechanism of transmission of 2019-nCoV has not yet been confirmed, it is expected to be by large respiratory droplets and direct or indirect contact with infected fluids. The potential for airborne transmission through unprotected exposure to aerosols of respiratory secretions or faeculant material may also exist. The transmission risk posed by asymptomatic carriers or patients in the initial stages of illness is not clear. In SARS-CoV the majority of human to human transmission events occurred after day five of illness.
While medical masks have been recommended and are reportedly selling out in China, there is limited evidence of benefit in community settings. Recommendations from WHO and national bodies re-enforce the importance of respiratory etiquette, hand hygiene and limiting hand contact with the eyes, nose and mouth.
International cooperation

A WHO delegation has just returned from a field visit to Wuhan and have reported high quality diagnostic, treatment and isolation services. Two 1,000-bed plus hospitals are currently being built in Wuhan to manage cases, and ventilatory capacity is clearly a key issue. The rapid sharing of genetic sequence and primers has facilitated countries to develop PCR diagnostic capability and WHO has issued emergency guidelines for case management. These are focused on optimised supportive care delivery, and, in the absence of proven therapeutics for coronaviruses, has recommended that unlicensed treatments are only evaluated in ethical, approved clinical trials or through the Monitored Emergency Use of Unregistered Interventions Framework (MEURI). A trial of lopinavir/ritonavir that has activity against coronaviruses is apparently being considered. The Coalition for Epidemic Preparedness Innovations (CEPI) has also announced that it is providing funding for three vaccine programmes against 2019-nCoV.
The world is certainly in a better place than it was during SARS in 2002, but the main risk remains the sustained transmission in China and spread to countries with weak health infrastructure. Disease outbreaks present a unique opportunity for collaborative research, and China’s transparency to date is hugely welcome. As cases increase and data emerges, the natural history of the disease will become clearer and WHO will meet again to review the PHEIC decision in the coming days. WHO and partners will be working to agree a name for 2019-nCoV recognising the previous controversy around MERS-CoV and other emergent pathogens. We are at a crucial juncture in the epidemic and now is the time that the world’s public health and industry/pharma expertise must come together to support China in controlling the epidemic. We must prepare and be ready to respond to cases in countries with reduced public health infrastructure and continue to recognise the immense efforts of healthcare workers on the frontline of this epidemic.