Adam Roberts is a Senior Lecturer and AMR lead at the Liverpool School of Tropical Medicine and the RSTMH Policy Advisor on Drug Resistant Infections.
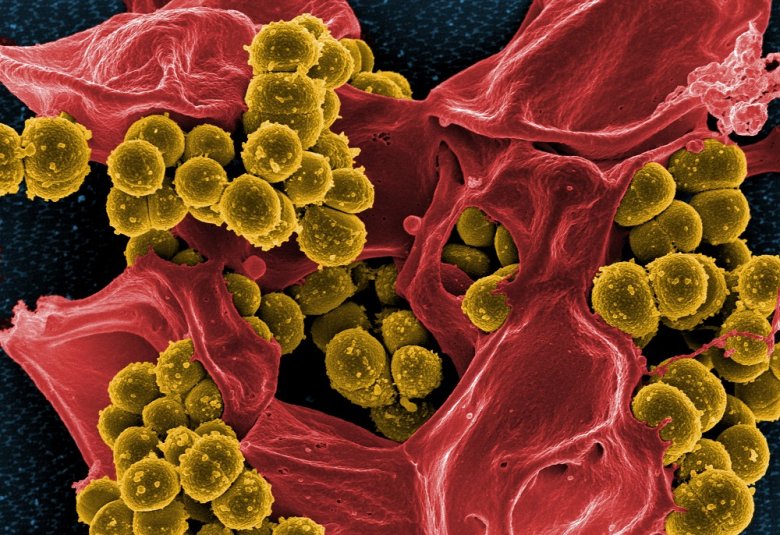
His research group is currently funded by the Medical Research Council (MRC) and the Biotechnology and Biological Sciences Research Council (BBSRC). The group is focused on investigating drug resistance in bacteria; particularly of low- and middle-income country origin, and the discovery and development of new drugs to treat bacterial and fungal disease.
It is appreciated that drug resistant infections (DRIs) are not as geographically constrained as their human, animal or plant hosts and that there are many countries and areas of the world where the effects of DRIs will be disproportionally felt due to limited resources and healthcare-infrastructure, as well as a reduced capacity and capability to monitor and respond to disease.
To limit the consequences of DRIs, a collective response is needed that similarly does not respect geographical and political boundaries.
International challenge of drug resistant infections
The international challenge of DRIs is increasingly illustrated by many national and international funding bodies highlighting it as a priority area of research, with an increase in collaborative opportunities to apply for support for investigations into both the problem of DRIs and potential solutions.
Recognition of the multi-disciplinary nature of DRIs is also increasing within the funding landscape and has had a transformative effect on the perception of the DRI problem, at least among many of those applying for funds to try and understand and fix it.
This is where RSTMH plays a key role. RSTMH membership maps well to the areas of greatest vulnerability from drug resistance.
The Society’s roles in terms of highlighting priority areas for research, education, dissemination of research findings via publications and advertising funding opportunities is also an important link between research groups, healthcare workers and clinicians, and policy stakeholders across the entire global One Health spectrum.
It is therefore with considerable enthusiasm that I look forward to working with the RSTMH as a policy advisor on DRIs as they move forward with their five-year strategic plan which places DRIs as one of their thematic priorities.
Global mortality due to fungal diseases exceeds that for malaria
Highlighting resistance in all pathogens, not just bacteria, is useful and necessary. Treatment of fungal disease, for example, is an increasingly challenging area of medicine due to antifungal drug resistance.
The global mortality due to fungal diseases exceeds that for malaria and is comparable to those for tuberculosis and HIV [1,2] which are also risk factors for fungal disease.
Drug resistance in all pathogens and vectors, needs to be kept on the political, funding and research agenda across all countries as the development of solutions, such as new drugs and diagnostics will take time.
There is no single quick fix for DRIs, as pathogens and vectors will continue to evolve and, therefore, so must our response.
If we do not address drug resistance in a particular group of organisms, we inadvertently provide them with an opportunity to flourish via our inactivity.
Failure to avoid this will increasingly become a problem for future generations to overcome.
References
1. Brown et al., 2012. Hidden killers: human fungal infections. Science Translational Medicine. 4(165):165rv13
2. Fisher et al., 2018. Worldwide emergence of resistance to antifungal drugs challenges human health and food security. Science. 360 (6390):739-742