HIV: A journey through adolescence
Rashida Ferrand is a Professor of International Health at the London School of Hygiene & Tropical Medicine. Since 2007, she has been based in Zimbabwe where she leads a research group conducting clinical and epidemiological studies on HIV infection in older children and adolescents. In 2018, she was awarded RSTMH’s Chalmers Medal for her work and delivered our Christmas lecture on this topic.
90% of the world’s adolescents with HIV are living in sub-Saharan Africa. The global scale-up of HIV prevention of mother to-child HIV transmission (PMTCT) programmes has resulted in a substantial decline in numbers of infants being born with HIV.
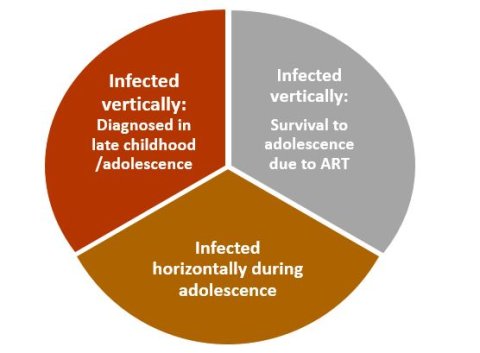
The concurrent scale-up of antiretroviral therapy (ART) programmes in the last decade has resulted in a dramatic increase in survival and children who would have otherwise died in early childhood are now surviving to adolescence and beyond.
In addition, a third of infants born with HIV have slow-progressing disease and as the HIV epidemic has matured, many of these slow-progressors are presenting for the first time with perinatally-acquired HIV in adolescence.
UNAIDS 90-90-90 targets
The UNAIDS has set ambitious 90-90-90 targets to end the HIV epidemic, whereby 90% of individuals with HIV will be diagnosed, 90% of diagnosed individuals will be on treatment and 90% of those on treatment will have viral suppression by 2020.
Not only are adolescents less likely to be diagnosed, but those who are diagnosed are less likely to access treatment and have lower rates of viral suppression once they start antiretroviral therapy.
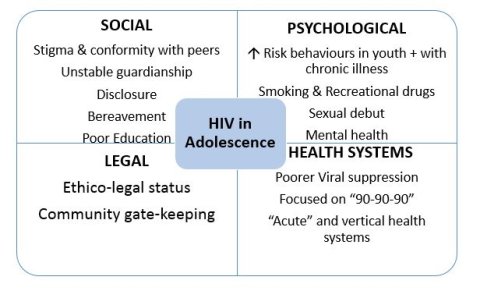
HIV testing is a critical gateway to accessing care and treatment, and barriers to HIV testing of adolescents include lack of awareness of risk of adolescents having perinatally-acquired HIV, prioritisation of PMTCT programmes, inadequate training of healthcare providers, the automatic disclosure of parental HIV status when a child is diagnosed and the requirement for consent from guardians for adolescents to undergo HIV testing when a large proportion of adolescents are orphaned and/or have unstable guardianship.
Promising strategies for HIV testing in this age-group include index-linked HIV testing, use of incentives and HIV self-testing.
Adherence to treatment lower in adolescence
As in other chronic diseases, adherence to treatment is lower in adolescence – a period when key life events take priority over managing one’s health. Correlates of poor adherence include lack of knowledge of one’s HIV status, mental health problems, burdensome ART regimens and poor treatment literacy, distance from clinics, stigma and in loco parentis caregiving arrangements.
The ZENITH trial conducted in Zimbabwe showed a significantly reduced odds in viral non-suppression among adolescents whose caregivers received community-based support, highlighting the critical role caregivers play in helping adolescents achieve optimal treatment outcomes. Other promising adherence strategies in the research pipeline include “weekends off treatment” and the use of long-acting injectable drugs.
The dramatic improvement in survival as a result of ART is undoubtedly a remarkable achievement. It is becoming increasingly apparent, however, that children reaching adolescence encounter a wide range of chronic complications of HIV infection, despite ART.
This may be due to the timing of infection (i.e. when the immune system has not fully developed) and/or delayed initiation of ART (the median age of ART initiation in children in Africa is around 8 years). These include growth failure (stunting and pubertal delay), cognitive impairment, chronic lung and cardiac disease, and skeletal disease which results in thinner bones, which may lead to premature risk of fragility fractures in later life.
HIV programmes in sub-Saharan Africa have, to date, largely focused on the 90-90-90 targets and hence many of these complications, which are difficult to diagnose and to treat, remain untreated and result in considerable disability.
Adolescents on ART will have at least a decade or longer exposure to ART than adults, and the consequences of the long term effects of ART exposure are not clear.
Psychosocial milieu
The psychosocial milieu in which adolescents with HIV live also deserves consideration. The HIV epidemic in sub-Saharan Africa has been accompanied by an “orphanhood epidemic”, which is also ageing, and therefore a large proportion of adolescents will have experienced bereavement, inconsistent care, loss of educational opportunities and having to provide care for siblings and ill family members, while dealing with their own illness.
Several studies have shown that adolescents with HIV are significantly more likely to be a school grade or more behind age-matched HIV-uninfected peers. School attendance is often interrupted due to illness, clinic visits, caring for ill relatives, economic hardship which contributes to poor educational outcomes.
At school, they experience bullying and exclusion from their peers. There is a high prevalence of psychiatric morbidity which is often not recognised.
Furthermore disclosure of HIV status to the adolescent is typically delayed and is often an abrupt and one-time event, so that many adolescents are growing up in a culture of silence about their infection. The consequences of this are far-reaching and adversely affect adherence to treatment, mental wellbeing and social adjustment, including family interactions and sexual relationships.
Transmission can be mother-to-child as well as sexual
Adolescents are the only age-group that can have acquired HIV infection through both mother-to-child as well as sexual transmission. Along with the cohort of children with HIV entering adolescence, this age-group also remains at very high risk of acquiring HIV infection through sexual transmission.
A third of all new HIV infections globally happen in 15-24-year-olds, the majority in sub-Saharan Africa: for example, in 2015 two-thirds of the global incident 250,000 infections in this age-group occurred in sub-Saharan Africa. The incidence in substantially higher in females, who are commonly infected by older males.
This is of grave concern given the substantial projected increase in the number of adolescents in sub-Saharan Africa in the next two decades (290 million adolescents by 2025) and the sub-optimal uptake and coverage of effective preventive interventions.
Targeting HIV prevention among adolescents is critical
While there has been a remarkable effort in addressing the HIV pandemic, much remains to be done.
Targeting HIV prevention among adolescents is critical given the persisting high incidence rates in this age-group. Adolescents are a particularly vulnerable group with disproportionately poor outcomes across the HIV care continuum and HIV programmes will have to focus on improving coverage of testing and treatment among adolescents if the ambitious UNAIDS targets are to be reached.
However, as the HIV epidemic matures, health systems will need to focus beyond virological outcomes if we are to help adolescents fulfil their potential and achieve health in its broadest definition.
