Leprosy – Continuing Challenges and A Hopeful Future
History of leprosy
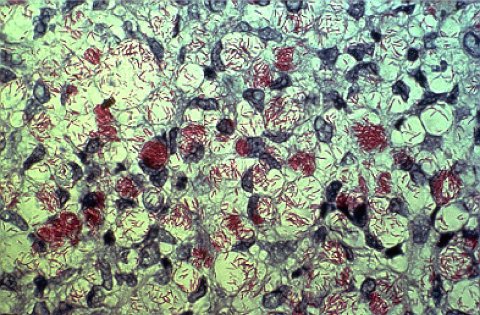
Leprosy is caused by the bacteria Mycobacterium leprae (M. leprae). Accounts of the disease can be found throughout history and people affected have often been stigmatised by their communities.
Leprosy is an infectious disease that causes skin patches and nerve damage in the eyes, arms, and legs. The infection is spread by the small number of infectious patients who cough and sneeze their mycobacteria into the environment. People then breathe in M. leprae and it settles in the nasal mucosa.
From the nose it moves to the immune system, skin and nerves. Most people’s immune system mounts an effective response to the mycobacterium and do not develop the disease. There is no simple diagnostic test for leprosy. The disease is diagnosed when the patient develops skin patches or damage to their peripheral nerves which manifest as tingling and numbness or weakness in their hands and feet.
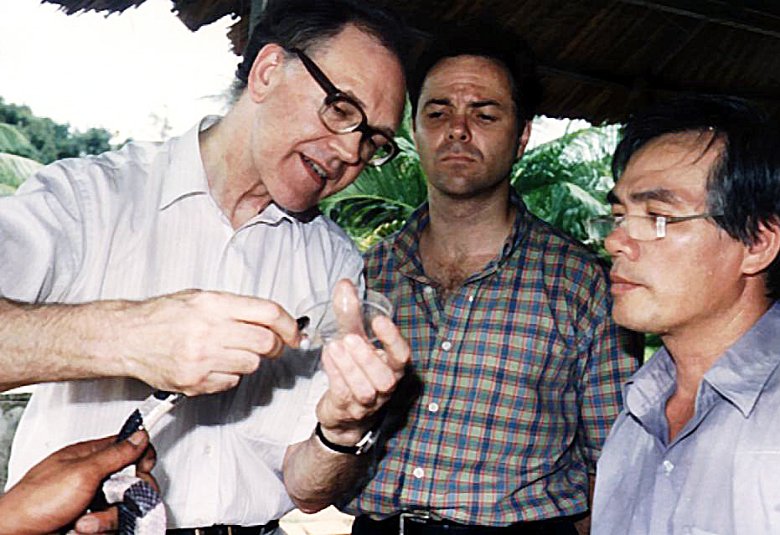
Patients are diagnosed with leprosy by finding these clinical signs or the presence of the mycobacteria on skin smears. The first effective antibiotic to treat M. leprae was Dapsone, discovered in the 1940s.
The World Health Organization has given important support for Neglected Tropical Diseases, of which leprosy is one, and supported leprosy activities through the Global Leprosy Programme. This introduced the worldwide free multi-drug therapy (MDT) in 1982, which comprise two or three antibiotics (Rifampicin and Dapsone and/or Clofazimine) that cures the leprosy infection when taken for 6 or 12 months.
Rifampicin is highly bactericidal for M. leprae when taken as a single monthly dose. This treatment has had a major effect in reducing the numbers of leprosy patients. Today the cure rate for leprosy is very high, 99% with a low relapse rate of 1%.1
Fortunately, there is no significant drug resistance of M. leprae to the MDT drugs, so treatment of patients diagnosed with leprosy can continue. The provision of free drug treatment has been an incentive to national leprosy programmes to detect patients with leprosy. In 1985, 550,224 patients were treated for leprosy.
Over the last eight years, the numbers of new cases have been stable at about 215,000 cases annually.3
The medication for leprosy was paid for initially by the Sasakawa Foundation and now the Novartis Foundation.
Complications

Leprosy patients can develop immune mediated inflammation of their nerves which results in nerve damage to their hands and feet. This puts them at risk of developing deformities. About 40% of leprosy patients will need a course of steroids to treat these immune mediated reactions.2
Huge challenges remain with leprosy because the disease, even when cured, leaves patients with chronic problems of nerve damage which can be lifelong. Many patients, despite being cured, have nerve damage even at the time of diagnosis. And this nerve damage can progress. Because people have anaesthetic hands and feet, they are at risk of injuring their extremities.
Care involves ensuring people have protective hand and footwear to prevent them from developing ulcers. Recognition of this is needed by patients, employers and families.
Psychological problems are also an important part of leprosy. Many patients are reluctant to share their diagnosis with family and friends, which may cause depression. Patients also often develop neuropathic pain experienced as tingling shocks in their skin, after treatment which is another chronic aspect of the disease.
The future of leprosy

Leprosy reduction should be seen as a marathon, not a sprint and it involves teams of people with many different skills. Diagnosing new cases will be a challenge as case numbers decline.
Dermatologists in the major leprosy endemic countries (India, Brazil, Indonesia, Nigeria) need to remain familiar with leprosy so they can recognise it and refer patients from their clinics. The management of leprosy complications such as reactions requires expertise in recognising and managing these phenomena.
The global effort for reducing stigma involves projects and campaigns to help people be seen as part of couples, families and their communities and not just their diagnosis.
Projects like the “New face for Leprosy”, which depicts people affected by leprosy living normal lives will help reduce this stigma.4
I hope for a future in which people will be treated for leprosy in regular dermatology clinics and will not experience stigma.
References
- WHO SEARO Leprosy
- Lockwood DNJ. Chronic aspects of leprosy-neglected but important. Trans R Soc Trop Med Hyg. 2019 Jan 31. doi: 10.1093/trstmh/try131
- C R Butlin & Lockwood DNJ Changing Proportions of paucibacillary leprosy cases in global leprosy case notification. Leprosy Review 2020 In press
- Lockwood DNJ, Bradley T New face for leprosy “A positive image for leprosy” Leprosy Review 2020, 91 2-13