District-level management of preventive NTD treatment – a personal story
Much progress has been made towards eliminating suffering caused by neglected tropical diseases (NTDs). Large scale preventive treatment interventions have been a leading catalyst for such progress.
One of the challenges for the WHO NTD Road Map 2030 is to spur integration of this intervention into routine health services. The progress achieved in terms of access to essential NTD medicines and WHO guidance for implementation has made this entirely possible.
First district assignment

I started my career as a medical doctor in Africa in the early 1980s. My first district assignment was to Rusape, Makoni district in Zimbabwe, about 200 km east of the capital Harare.
Urinary schistosomiasis (or bilharzia) was a public health problem in that area. I did not need to conduct a burden assessment to realise that – on one of the first days of my assignment a delegation of school headmasters came to my office complaining that most pupils were urinating blood, the characteristic sign of the disease. As the health expert in the district, I had to solve the problem.
The means available to me were limited. There was metrifonate for the treatment of urinary bilharzia, and there were hemastix reagent test strips, to detect blood in urine when it was not directly visible.
Hemastix were rather expensive, but I was able to double the amount by cutting them in half, and I was able to find affordable, locally produced, and reusable plastic containers for urine collection.
Test-and-treat

Each of the health centres in the district had approximately 20 primary schools in their catchment areas. They were staffed with a medical and a health assistant, the latter being equipped with a bicycle and responsible for outreach activities.
So, I asked the health assistants to go and visit each school in their catchment area at least once a year, ask the pupils to provide a urine specimen and test the non-bloody urines with hemastix. All those with visible blood in their urine or microscopic haematuria, as diagnosed by a test strip, were treated with a single dose of metrifonate (10 mg/kg body weight).
Although the metrifonate product leaflet recommended repeating the treatment twice at fortnightly intervals, haematuria disappeared rapidly after a single dose. Moreover, the health assistants knew the “hot spots” of bilharzia where they needed to go and test-and-treat more frequently than once per year to keep the situation under control.
As a result of these interventions, haematuria among primary school children disappeared in the district. Still, the programme could not be stopped because of ongoing intense transmission of the disease, as indicated by the tenaciously high levels of haematuria in children entering grade 1 each year.
I would have loved to also deworm all children systematically with mebendazole, but at the time I could not afford the recommended dose, which in this circumstance was five 100mg tablets for all children.
I therefore introduced what would later be called “treatment holidays” and rotated schools for mebendazole treatment with what I could afford on my district health budget.

When I had the opportunity to go and work for WHO in 1998, I realised that several of my colleagues had had similar experiences in the field and were as motivated as I was to finding global solutions to facilitate the control of local tropical disease priorities.1
The convergence of those people to what was then called the WHO Department of Control of Tropical Diseases (CTD) has been at the origin of WHO’s current NTD strategy and progress towards eliminating the suffering caused by NTDs.
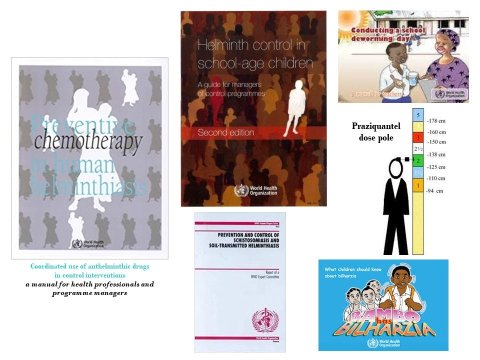
Indeed, if I had to revisit my district implementation scenario today, my task would have been considerably easier. First, I would not have had to figure it out by myself - there would have been clear WHO guidance on how to go about it.
Rather than test-and-treat, I would have asked the public health nurses in the district to carry out an initial survey that could have been combined with one of the vaccination coverage surveys they were doing routinely. They could have used the same reagent test strips or more cumbersome, but less expensive urine filtration. And we would have decided on treatment strategies for the various parts of the district according to WHO recommendations. There would have been no limitations in available quantities of medicines2 and the health assistants could have used a dose pole,3 not needing fragile weighing scales anymore to dose the medicines.
I could have requested, through the national system,4 the quantities of donated praziquantel (that is more efficacious than metrifonate) and mebendazole 500 mg or albendazole 400 mg to treat all children in need, without having to leave any behind.
Looking back
In terms of implementation, I could have used the same system as before – asking health assistants or their equivalent today to go to schools in their catchment area, or I could have introduced district-wide “deworming days” once or twice per year involving primary school teachers for the delivery of the preventive medicines. The frequency of treatment would have been tailored to the local need through a routine yearly implementation system.
For example, two-yearly treatment for bilharzia would have translated into treatment of pupils with praziquantel in grade 1, 3 and 5 during one of the deworming days every year – so that children going through their primary schooling cycle would get treatment every other year. I cannot emphasise enough the advantages of setting up a routine system of school- or community-based treatment that is carried out year-by-year and in which the frequency of treatments can be tailored to a given situation, as compared to a more intermittent “vertical” system of implementation that is less sustainable and logistically more difficult to organise.
Like what has been achieved in terms of simplification of anti-retroviral treatment for HIV and AIDS in peripheral health services, the normative work of WHO has facilitated the potential for implementation of large-scale preventive treatment at the district level. The immense progress we see today would have never happened without a strong programmatic focus globally, as exemplified by WHO’s 2020 NTD roadmap, the London Declaration, and the gathering of partners around them.5
That must continue. Yet, with the currently available guidance tools and free medicines, implementation at the district level is possible if health personnel are adequately skilled through their basic training curriculum. There is nothing complicated about it, and implementation costs are affordable on most district health budgets.
The key to success, therefore, lies in national health policies being favourable to the inclusion of NTDs as local priorities in the Universal Health Coverage package and the systematic building of health workforce capacity to deal with them.
District health teams today are no different from the ones I have worked within the early 1980s. With the normative guidance and facilities available for NTDs today, they are bound to do better than we did at the time.
References
Engels D, Zhou X. Neglected tropical diseases: an effective global response to local poverty-related disease priorities. Infect Dis Poverty 9, 10 (2020). https://doi.org/10.1186/s40249-020-0630-9
World Health Organization. Essential medicines donated to control, eliminate, and eradicate neglected tropical diseases. https://www.who.int/neglected_diseases/Medicine-donation-04-march-2019.pdf?ua=1. Accessed 28 July 2020.
Montresor A, Engels D, Chitsulo L, Bundy DA, Brooker S, Savioli L. Development and validation of a 'tablet pole' for the administration of praziquantel in sub-Saharan Africa. Trans R Soc Trop Med Hyg. 95(5):542-544 (2001); https://doi.org/10.1016/S0035-9203(01)90034-3
World Health Organization. Preventive chemotherapy for neglected tropical diseases – planning, requesting medicines, and reporting. https://www.who.int/neglected_diseases/preventive_chemotherapy/reporting/en/ Accessed on 28 July 2020
Uniting to Combat NTDs - in support of the WHO NTD roadmap and the London Declaration. https://unitingtocombatntds.org/about-us/ Accessed on 28 July 2020