Leprosy - pioneering women in past, present and future
Leprosy is caused by the bacteria Mycobacterium leprae (M. leprae). Accounts of the disease can be found throughout history and people afflicted have often been ostracized and stigmatised by their communities.
Leprosy is an infectious disease that causes skin patches and nerve damage in the eyes, arms, and legs. The first effective antibiotic was dapsone, discovered in the 1940s. Treatments today comprise effective multi-drug-therapies, with shorter treatment courses (now on average between 6-12 months) [1].
Leprosy is an important Neglected Tropical Disease with approximately 200,000 new confirmed infections each year [1]. The loss of sensation that is so characteristic of leprosy may be a life-long problem for patients and keeping the patents’ limbs intact for a lifetime remains a challenge for patients, their families and health workers.
Since the 20th century, treatments for leprosy and associated disabilities have been worked on by many outstanding scientists, including pioneers Ms Jean Watson, Professor Indira Nath and RSTMH members, Professor Diana Lockwood and Dr Saba Lambert.
Jean M Watson

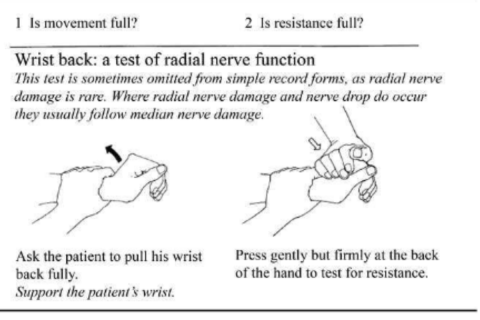
Jean Watson was a chartered physiotherapist and hydro therapist. She had a longstanding interest in leprosy and received her first formal training in the disease in Karigiri, India, in 1960-1961. During the 1960s Jean served as a physiotherapist in Hong Kong, Malaysia and Australia where she managed activities of establishing departments of physiotherapy for leprosy patients and training large numbers of staff in the prevention and management of disabilities. Her line drawings which aided the assessment of patients and were developed in the 1960s, are still used in handbooks, assessment guides and literature. [2]
From 1972, Jean worked at the renowned All-Africa Leprosy and Rehabilitation Training Centre (ALERT) in Addis Ababa, Ethiopia, as Chief of Physiotherapy. She was responsible for the management of the local disabled leprosy patients and trained many hundreds of leprosy workers from all over Africa. She also taught and gave workshops on the management of the leprosy-disabled patient in many other countries in Africa.[2]
From 1979 to 1995 she was a Physiotherapist Consultant at The Leprosy Mission international, advising on priorities and methods in the management of disability and the rehabilitation of leprosy patients and those disabled from other causes. [2]
Indira Nath
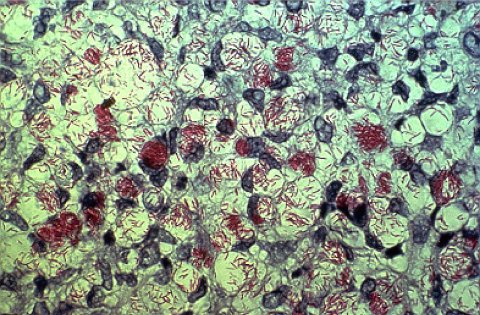
Professor Indira Nath is an Indian immunologist and pathologist, focusing on the mechanisms underlying immune unresponsiveness in men, reactions and nerve damage in leprosy and a search for markers for viability of the Leprosy bacillus.
After hospital training undertaken in UK in the late 1960s, she returned to the All India Institute of Medical Sciences (AIIMS) for her MD in Pathology and specialised in immunology. She decided to work in the area of infectious diseases, particularly leprosy which was a major concern in India at that time.[3]
Indira Nath made pioneering contributions to immunology research by her seminal work on cellular immune responses in human leprosy. Throughout a career of over 30 years, her research contributions led to the creation of tools for diagnostics, immunotherapy and antigens for clinical investigations.
She founded and established the Department of Biotechnology at AIIMS, and continues to mentor many MBiotech, MD and PhD students in her retirement.
Diana Lockwood

Professor Diana Lockwood became interested in leprosy on a gap year in India in 1975, when she volunteered at a South Indian leprosy hospital. She saw that leprosy was an interesting disease with many potential interventions that could improve people’s lives. She travelled home overland through Pakistan, Afghanistan, Iran, Turkey and Europe. She trained in medicine at the University of Birmingham in 1981, then focused on infectious diseases and specialised in tropical medicine, researching leprosy from 1988 at the London School of Hygiene & Tropical Medicine. She was appointed a leprologist and the first female consultant with the NHS (Hospital for Tropical Diseases). She also had an academic post at the London School of Hygiene & Tropical Medicine in 1994, becoming a professor in 2007 until her retirement in 2019. She worked in India, Ethiopia and across the globe.
Focusing on understanding the pathogenesis of reactions and immunology of leprosy reactions, she set up randomized controlled trials to improve the treatment of leprosy reactions. She identified neuropathic pain as an important complication of the disease. She set up the global multi-centre ENLIST collaboration, an international partnership between seven countries focused on improving the understanding and treatment of Erythema nodosum leprosum (ENL). At the Hospital for Tropical Diseases she ran the leprosy clinic with a unique cohort of 150 patients with imported leprosy.
Her new project, called “New Face for Leprosy” aims to improve the image of leprosy by showing people with leprosy living normal lives, working and having families.
Diana has joined the RSTMH Board of Trustees in September 2019 and continues to mentor the next generation of researchers on leprosy. She learnt Hindi in 2005 and has cycled across Tibet and on 4 continents, writing about her travels in her blog.
Saba Lambert

A new generation of leprosy researchers are now taking the baton. Among them, RSTMH member Dr Saba Lambert, leprosy clinician in Addis Ababa at the All Africa Leprosy, Tuberculosis and Rehabilitation Training Centre (ALERT). She grew up in Ethiopia and fled during the communist period to Zimbabwe where she spent her teens. After she trained in medicine at Dundee University, Scotland, she worked in Zimbabwe, South Africa and New Zealand before returning to Scotland as a GP on the island of Arran.
Her interest in leprosy was sparked when Diana showed a picture of the beautiful Ethiopian highlands during a lecture on the Diploma in Tropical Medicine course in Liverpool. As Diana talked about the challenges of researching leprosy, she mentioned she was looking for people to work in leprosy, Saba was inspired and joined Diana’s team at LSHTM in 2010 as a PhD student. She led the team on several trials at ALERT in Addis Ababa, working with leprosy patients with reactions to determine whether the drug ciclosporin would improve the inflammation in patients’ skin and nerves. Most of the patients completed this study, thanks to Saba’s patient-focussed approach. During the trial she kept a close watch on patients, even giving them her mobile number so they could report any problems. This important negative study showed that leprosy associated inflammation is difficult to switch off.
She is a vital member of the ENLIST team, working in the only African research centre in the consortium. She was also a key member for the New Face for Leprosy project in Ethiopia, working with patients and ensuring their central role in the project.
“I am grateful to have had a mentor like Professor Diana Lockwood, an adventurous and thoughtful woman, who has encouraged her younger female colleagues to work meticulously, aim higher and maintain interests outside medicine. She awoke in me a passion for this ancient, misunderstood and neglected disease which has so many aspects that are yet to be addressed. I don’t think leprosy is anywhere near elimination, and with so many unanswered questions, and ongoing numbers of new patients affected by leprosy, I have years of work ahead of me to do!”
References
[1] Leprosy. (n.d.). https://www.who.int/news-room/fact-sheets/detail/leprosy
[2] News and notes. Int. J. Lepr. 1998;66(4):490-5
[3] Birmingham, K. Indira Nath. Nat Med 8, 545 (2002). https://doi.org/10.1038/nm0602-545
[4] Indian Fellow Detail. (n.d.). http://insaindia.res.in/detail/N92-1095