Still neglected? Progress and challenges discussed at neglected tropical disease summit
From 18–22 April 2017, a series of events were held in Geneva, Switzerland, creating a neglected tropical diseases (NTD) summit.
Ministers of Health from NTD endemic countries, together with their delegations, UN organisations (particularly the WHO), chief executive officers (CEOs) of major pharmaceutical companies, major governmental and non-governmental donors, implementing partners and specialists in public health, and particularly NTDs, all met together over four days to discuss progress, common challenges and the way forward, looking initially to 2020 and then further towards 2030 and sustainable development goals (SDGs).
It has been 10 years since the first Global Partners Meeting, sponsored by the WHO, and five years since the same key partners met at the major NTD event that led to the London Declaration, highlighting 10 diseases where it was thought significant progress could be made towards elimination by 2020.
This meeting led to the creation of a coordinating organisation, Uniting to Combat NTDs (UTC), which, working with the WHO, organised this event. The purpose of the London meeting was to gather support to combat NTDs and to develop the WHO guide for what needed to be done in the NTD Road Map for implementation.
WHO neglected tropical diseases list
- Buruli ulcer
- Chagas disease
- Dengue and chikungunya
- Dracunculiasis (guinea-worm disease)
- Echinococcosis
- Foodborne trematodiases
- Human African trypanosomiasis (sleeping sickness)
- Leishmaniasis
- Leprosy (Hansen’s disease)
- Lymphatic filariasis
- Mycetoma, chromoblastomycosis and other deep mycoses
- Onchocerciasis (river blindness)
- Rabies
- Scabies and other ectoparasites
- Schistosomiasis
- Soil-transmitted helminthiases
- Snakebite envenoming
- Taeniasis/cysticercosis
- Trachoma
- Yaws (endemic treponematoses)
The donation of Mectizan® (ivermectin) by Merck & Co. 30 years ago has now mushroomed into massive donations from major (and smaller) pharmaceutical companies of medications for many of these neglected diseases, including albendazole by GlaxoSmithKline for both lymphatic filariasis (LF) and soil-transmitted helminths, Zithromax (azithromycin) for trachoma by Pfizer and multidrug treatment for leprosy by Ciba Geigy (now Novartis), among others.
Partners meet around the same table to coordinate their donations together with funding organisations, who in turn are working with countries and non-governmental organisations to deliver preventive chemotherapy and other specific medical treatments to populations in need.
NTDs not just about medicines
NTDs not just about medicines
NTDs are not all about swallowing medicines. Patients suffering from some of these diseases (e.g., LF and leprosy) suffer significant disabilities and need longer term patient management. Other diseases (e.g., soil-transmitted helminths [STHs], schistosomiasis and trachoma) need water, sanitation and hygiene activities (WASH), combined with drug treatment, if gains are to be maintained and transmission controlled, which will hopefully also increase the impact of medicines at the community level. Efforts are needed to prioritise and coordinate research.
On 18 April 2017, CEOs met with Bill Gates and others at a CEO roundtable to review progress and look at gaps in donations of medicines and diagnostics that could advance the progress of NTD elimination.
This was followed by a series of panels where different leaders were asked about their contributions and ongoing commitment. The panels were interspersed with presentations highlighting progress so far. This set the scene for the Global Partners Meeting at the WHO headquarters the following day.
On 19 April 2017, the Global Partners Meeting took place at WHO headquarters in Geneva. The theme was ‘Collaborate, Accelerate and Eliminate’. This was also the occasion when WHO presented its fourth NTD report entitled ‘Integrating neglected tropical diseases in global health and development’.
The meeting was chaired by the director-general of the WHO. Several ministers of health came from endemic countries and made it clear that not only did they want to move ahead with NTD elimination, but they were also ready to put some national resources into the programme.
The pharmaceutical industry was very evident and new commitments were made to support activities with drug donations. Major donors were present and commitments were made to support NTD elimination, including a pledge from the Department for International Development (DFID) of £360 million towards implementation programmes to tackle NTDs between 2017–18 and 2021–22.
Non-governmental development organisations (NGDOs) also committed themselves to assisting with funding and implementation to try and achieve these goals.
In summary, pledges of more than US$800 million were made over the next 5–7 years to accelerate the elimination and eradication of NTDs.
A major event on the evening of 19 April 2017 was a reception honouring women involved in NTD work, representing community activists and women involved at all different levels of implementation.
Strategies for tackling NTDs and achieving SDGs
The last three days of the summit were disease-specific, with more than 600 people present. This was the first time when so many disease groups had come together and, despite being disease-specific, there were crossover issues that were addressed for all attendees and between specific groups where appropriate. The NTD NGDO Network, commonly known as NNN, has been bringing together organisations working with governments helping with both implementation and funding.
As patient care develops and other crossover issues become more evident, the NNN has proposed the BEST strategy (Behaviour, Environment, Social Inclusion and Treatment). The details can be found on their website, but this more comprehensive way of approaching NTDs and achieving SDG goals was explained to the wider group in a plenary session.
There were further plenary sessions on WASH and patient management, including morbidity management and disease prevention (MMDP) and disease management and disability inclusion (DMDI). For some disease groups, for example, Chagas disease and leishmaniasis, this was the first time such a meeting had been held, at least with a wider group.
Other groups have been meeting regularly, but this was an occasion to look at specific issues related to implementation, elimination strategies, monitoring and evaluation.
As LF is eliminated in various parts of the globe and interventions cease (the most effective STH control programme globally), there is a need to start an STH-specific programme, but what strategy would be best? Onchocerciasis elimination and LF elimination need to work together in many parts of Africa. How do you do combine implementation? How do you decide to stop treatment for one of the diseases when treatment continues using the same medication? How should schistosomiasis control and STH work together to create efficiencies and achieve suitable control/elimination strategies?
The full report will be available in the near future and the details will be available on the Uniting website.
Diseases of neglected people
There has been a lot of success to report, a lot of renewed commitment in terms of funding, particularly domestic funding, and a lot of working together on efficient implementation, including crossover issues. Patient behaviours, patient care and environmental factors are now being included as programmes develop.
Endemic countries are realising the importance of NTDs and their control or elimination as indicators of health provision. However, these are diseases of neglected peoples. Often poorer and more remote populations have little economic impact, no political power and are not counted as important, particularly by ministers of finance who need to mobilise domestic funding.
Robust NTD programmes can strengthen the health systems from the bottom up, as populations are involved in their own decision-making and as efforts are made to break the cycle of poverty. Effective NTD implementation can ensure no one is left behind and be a major factor for achieving SDG 3.3 in health.
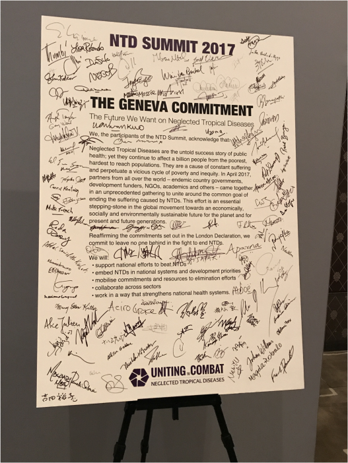
The participants signed a pledge of on-going commitment to the goals of 2020 and the SDGs in 2030. Is there a broader national and international will to achieve major, but low-cost, highly effective interventions to help achieve these goals?